When Hunger Signals Lose Their Rhythm
Appetite is not the enemy. I want that clear from the start. Hunger is a sophisticated conversation between your gut, brain, hormones, nerves, and even your emotional state. When it works well, you eat, feel satisfied, and move on with your day. When it loses rhythm, everything feels louder. Cravings shout. Fullness whispers. You eat without meaning to, or you forget to eat until your body crashes. This is where most people start looking for herbs for appetite control, not because they want to fight hunger, but because hunger stopped making sense.
Modern life disrupts appetite in subtle ways. Irregular meals. Chronic stress. Ultra-processed foods are designed to bypass satiety signals. Sleep that never quite restores the nervous system. Over time, the body forgets how to read its own cues. Ghrelin rises when it should fall. Leptin resistance creeps in quietly. Blood sugar spikes and drops shape hunger more than actual energy needs. Appetite becomes reactive instead of responsive.
Table of Contents
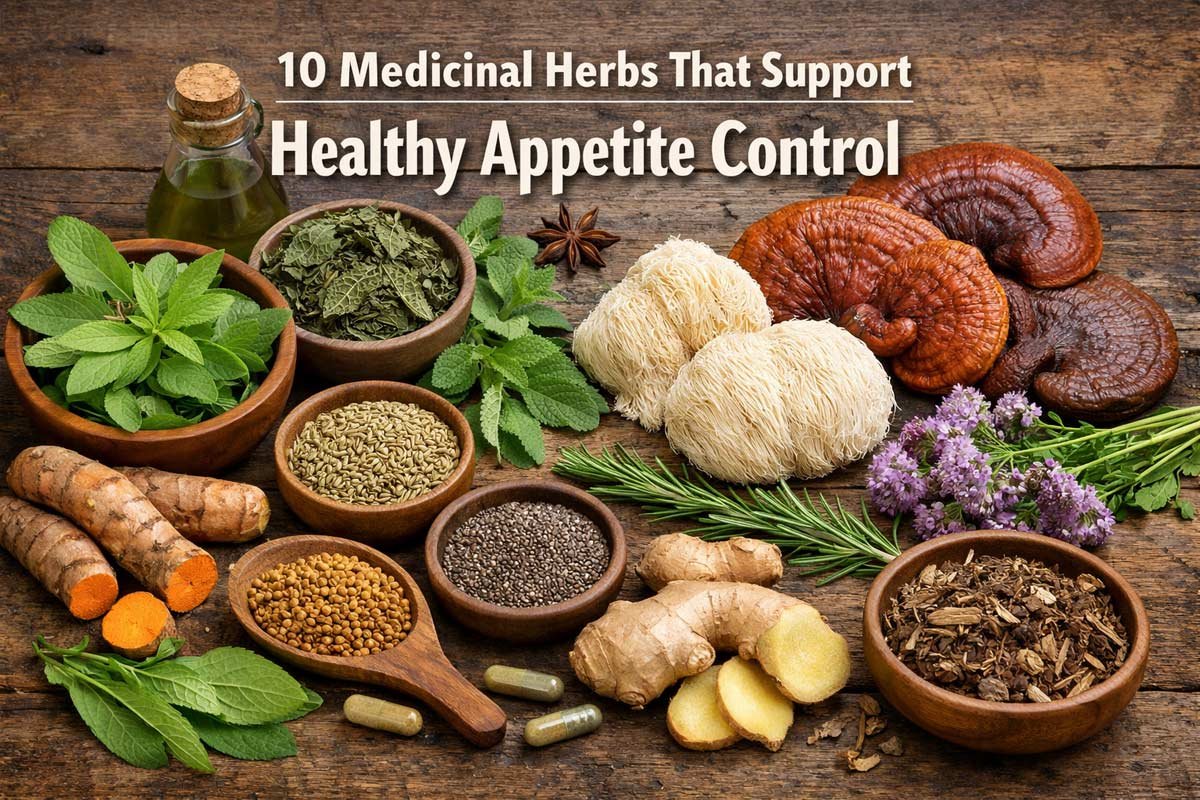
Traditional herbal medicine never approached appetite as a willpower issue. It was always about restoring communication. When I look at classic systems like Ayurveda, Traditional Chinese Medicine, and European folk herbalism, appetite regulation shows up everywhere. Bitter roots before meals. Aromatic seeds after eating. Mushrooms used to steady the nervous system rather than suppress desire. The goal was never to shut hunger down. It was to bring it back into tune.
Herbs for appetite control work because they interact with real physiological pathways. Some slow gastric emptying, allowing fullness to register. Some influence insulin sensitivity, which changes how quickly hunger returns. Others calm the stress response, reducing emotional eating without touching digestion directly. A few even alter taste perception, making overly sweet foods less compelling. None of this is magic. It is chemistry meeting biology, guided by centuries of observation.
One of the most misunderstood ideas around appetite is that it lives only in the stomach. In reality, appetite begins in the brain, long before food reaches the gut. The hypothalamus integrates signals from hormones, nutrients, and nerves. Stress hormones like cortisol can override satiety. Dopamine pathways tie food to reward and comfort. This is why appetite often intensifies during emotional strain, even when the body has enough fuel. Herbs that support appetite balance often work by calming these neural loops, not by blocking hunger signals outright.
Digestion also plays a central role. If digestion is weak, appetite becomes erratic. You may crave food constantly because nutrients are not absorbed efficiently. Or you may feel full quickly but hungry again an hour later. Bitter herbs were traditionally used to stimulate digestive secretions, not to increase appetite blindly, but to improve digestive efficiency so appetite could normalize. In that sense, herbs for appetite control often look like digestive tonics rather than suppressants.
Blood sugar deserves attention here. Rapid spikes followed by sharp drops drive intense hunger that feels urgent and non negotiable. This is not lack of discipline. It is physiology. Several herbs used for appetite regulation slow carbohydrate absorption or improve glucose handling. When blood sugar stabilizes, appetite softens naturally. Meals feel complete. Snacking loses its grip. This is one of the most reliable ways herbs for appetite control support long term balance.
Then there is the nervous system. Chronic sympathetic activation keeps the body in a state of perceived scarcity. Eat now. Eat more. Store energy. This pattern made sense in evolutionary stress. It does not serve modern life. Adaptogenic herbs and medicinal mushrooms help shift the body out of this constant alert mode. When the nervous system settles, appetite follows. You start eating because you are hungry, not because you are tense or tired.
Taste also matters more than most people realize. Overexposure to intense sweetness and salt dulls natural taste receptors. Mild foods stop satisfying. Certain herbs temporarily reduce sweet taste perception or enhance bitter sensitivity. This changes food choices without effort. People often notice they stop craving desserts after meals or feel satisfied with simpler foods. This is a gentle but powerful form of appetite regulation.
I want to be clear about expectations. Herbs for appetite control do not override biology. They do not erase hunger overnight. What they do is create conditions where hunger can behave like hunger again. Predictable. Appropriate. Proportional. That process takes time. The body needs repetition and consistency to trust new signals. Herbs support that retraining.
Another point that deserves honesty is that appetite issues rarely exist alone. They often sit alongside fatigue, poor sleep, digestive discomfort, or mood fluctuations. This is why single compound solutions fail. Herbal medicine works best when it addresses patterns, not symptoms. Appetite becomes balanced as a side effect of broader regulation.
In my experience, the people who benefit most from herbs for appetite control are those willing to observe themselves. How hunger changes with stress. How certain foods trigger more eating. How sleep alters cravings. Herbs amplify awareness as much as they alter chemistry. You start noticing the difference between hunger and habit. Between fullness and fatigue. That awareness is part of the medicine.
There is also a cultural shift that needs addressing. Appetite suppression has been marketed as success. Feeling less hunger is framed as progress. From a physiological standpoint, suppressed appetite often signals imbalance. True regulation feels different. Hunger arrives calmly. Eating feels grounding. Fullness brings clarity, not heaviness. Herbs used wisely move you toward that state.
This article focuses on plants and mushrooms with documented effects on appetite regulation. Not folklore alone. Not trends. These are herbs for appetite control supported by traditional use and modern research. Some act on glucose metabolism. Some influence satiety hormones. Some work through the gut brain axis. Others steady the nervous system so appetite can settle on its own.
If your hunger feels chaotic, it is not because you are broken. It is because the signals got scrambled. Herbs do not force obedience. They restore conversation. When that conversation resumes, appetite stops being something you fight and starts being something you trust again.
Herbs That Influence Hunger and Satiety Hormones
When appetite feels out of control, hormones are usually involved. Hunger and fullness are not abstract sensations. They are driven by messengers like ghrelin, leptin, insulin, and peptide YY. These signals rise and fall in response to food, stress, sleep, and blood sugar. When they lose coordination, appetite becomes distorted. This is where some of the most reliable herbs for appetite control show their strength, not by numbing hunger, but by changing how these signals behave.
I tend to think of this group of herbs as negotiators. They step into biochemical conversations that have become one sided. Instead of telling the body to stop eating, they influence how strongly hunger is perceived, how quickly satisfaction arrives, and how long it lasts. Used consistently, they help appetite feel proportional again.
1. Gymnema sylvestre
Gymnema has a reputation that borders on myth. Chew the leaf and sweetness disappears. Sugar tastes flat, almost meaningless. That alone tells you something important. Appetite is deeply tied to taste perception, especially sweetness. When sweetness loses its pull, cravings often soften without effort.
But Gymnema does more than play tricks on taste buds. Research shows it influences glucose metabolism and insulin activity. By improving how cells respond to glucose, it reduces the sharp blood sugar swings that trigger intense hunger. When blood sugar stabilizes, ghrelin does not spike as aggressively. Appetite becomes calmer and less urgent.
What I notice most with Gymnema is how it changes relationship to sweet foods. People stop chasing dessert after meals. Snacking becomes optional instead of compulsive. This is not suppression. It is recalibration. The brain stops lighting up every time sugar appears.
Gymnema earns its place among herbs for appetite control because it addresses both ends of the problem. It reduces the sensory reward of sweetness and supports metabolic signals that influence hunger timing. It works best when used regularly, not as a one time fix. Over weeks, taste preferences often shift naturally.
2. Fenugreek (Trigonella foenum-graecum)
Fenugreek seeds are humble, sticky, and surprisingly powerful. When soaked or cooked, they release soluble fiber that slows digestion. This physical property matters. Slower gastric emptying means fullness signals have time to register. The gut sends peptide YY and GLP one more steadily. Hunger stays quieter for longer.
Fenugreek also improves insulin sensitivity. Multiple studies show reduced post meal glucose spikes when fenugreek is included. This is one of the most practical mechanisms herbs for appetite control can offer. Stable blood sugar equals fewer hunger crashes.
There is also something grounding about fenugreek. It has weight. Texture. Warmth. It feels nourishing rather than restrictive. People often report feeling satisfied sooner and staying full longer, without feeling deprived. That matters psychologically. Appetite regulation fails when it feels punitive.
Fenugreek shines for those who feel hungry again too soon after eating. Especially after carbohydrate heavy meals. It slows the whole process down, allowing satiety hormones to do their job. Over time, meal size often decreases naturally, not because of effort, but because enough finally feels like enough.
3. Garcinia cambogia
Garcinia has been marketed aggressively, often poorly, and that has done it no favors. Stripped of hype, it has a specific and limited role. The active compound hydroxycitric acid influences fat metabolism and may modestly affect appetite through serotonin pathways.
Serotonin plays a role in satiety and emotional eating. Low serotonin activity often correlates with increased appetite and carbohydrate cravings. Garcinia appears to increase serotonin availability, which can enhance feelings of satisfaction after eating. This effect is subtle, but noticeable for some.
It also inhibits an enzyme involved in fat synthesis. While this is often discussed in weight loss terms, it has indirect appetite effects. When energy metabolism shifts, hunger signals can adjust accordingly. That said, Garcinia is not a standalone solution. Its effects are context dependent.
Among herbs for appetite control, Garcinia works best for people whose appetite feels tied to mood and reward. Emotional eating. Late night cravings. Restless snacking. It does not suppress hunger directly. It changes the emotional tone around eating. When satisfaction increases, the urge to keep eating fades.
Used thoughtfully, Garcinia can support appetite regulation, but it should never be framed as a miracle. It works best alongside dietary consistency and nervous system support.
4. Caralluma fimbriata
Caralluma is less known, but deeply interesting. Traditionally used in regions where food scarcity was common, it was valued for reducing hunger during long hunts or travel. Modern research suggests it influences appetite related neuropeptides in the brain.
Specifically, Caralluma appears to reduce ghrelin signaling. Ghrelin is often called the hunger hormone, but it is more accurately a meal initiator. When ghrelin stays elevated, hunger feels constant. Caralluma helps quiet that signal.
What stands out with Caralluma is that it reduces appetite without stimulating the nervous system. No jitteriness. No rebound hunger. Appetite simply feels less demanding. People describe feeling indifferent to food between meals, which is rare.
This makes Caralluma one of the more direct herbs for appetite control. It does not rely heavily on digestion or blood sugar alone. It acts centrally, influencing how hunger is perceived. That makes it useful for those who feel hungry even when nutritional needs are met.
However, it should be used with intention. Appetite suppression without nourishment leads to imbalance. Caralluma works best when meals are regular and nutrient dense. In that context, it helps appetite align with actual need rather than constant signaling.
Taken together, these herbs illustrate an important point. Appetite regulation is not about force. Each of these plants nudges a different lever. Taste perception. Blood sugar stability. Satiety hormones. Neurochemical reward. When combined thoughtfully, they create a steadying effect.
Herbs for appetite control are most effective when they match the pattern. Sweet cravings point toward Gymnema. Rapid hunger return suggests Fenugreek. Emotional eating may respond to Garcinia. Constant hunger without cause often benefits from Caralluma. Listening matters more than stacking everything at once.
When hunger hormones fall back into rhythm, eating becomes simpler. You stop negotiating with yourself. You eat, you stop, you move on. That is not discipline. That is physiology doing what it was designed to do.
Digestive and Metabolic Herbs That Shape Appetite Cues
Appetite does not start in the brain alone—it begins in the gut. Digestion and metabolism send continuous feedback to hunger centers, modulating how full or hungry we feel. If the gut is sluggish, bloated, or imbalanced, appetite signals can misfire. This is where digestive and metabolic herbs come into play. They don’t force restraint; they optimize internal processes so the body can naturally know when to eat and when to stop. Among herbs for appetite control, some of the most potent work along these digestive and metabolic pathways, subtly influencing satiety, blood sugar, and nutrient absorption.
These herbs are practical allies. They are not about suppression, but refinement. They improve the quality of the signals your body sends and receives, making hunger proportional, timely, and reliable. Let’s look at three that have stood the test of both tradition and modern research.
5. Ginger (Zingiber officinale)
Ginger is a kitchen staple, but its impact on appetite is sophisticated. Beyond its familiar warming and spicy notes, ginger stimulates gastric motility and digestive secretions. By encouraging food to move efficiently through the stomach and small intestine, it allows fullness signals to reach the brain at the right time. A slow or inefficient digestive process can distort satiety, making you feel hungry even after eating enough. Ginger helps restore that timing.
Ginger also has thermogenic properties, slightly raising metabolic rate. This doesn’t burn off calories in a dramatic sense, but it improves energy utilization, which indirectly influences hunger patterns. When metabolism is steady, cravings tend to normalize. People often report that including ginger before or during meals reduces the compulsion to snack later.
Another underrated effect of ginger is its ability to soothe the digestive tract. Minor inflammation or discomfort in the stomach can trigger vague hunger or cravings for easily digestible, often carbohydrate-rich foods. Ginger reduces that subtle irritation, letting true appetite shine through. In traditional medicine, it’s been used for centuries as a digestive tonic precisely for this reason, long before anyone studied hormones or neurotransmitters.
The best way to use ginger for appetite support is simple: fresh slices in warm water, grated into meals, or as a lightly brewed tea. The dose is less important than consistency. Over time, it retrains the gut-brain axis, making appetite cues clearer.
6. Green Tea (Camellia sinensis)
Green tea occupies a unique niche among herbs for appetite control because it works through multiple systems. Its active compounds, catechins, influence glucose metabolism and insulin sensitivity. Blood sugar spikes become less pronounced, meaning hunger after meals is less abrupt and intense. When insulin levels are more stable, ghrelin surges are moderated, which smooths appetite throughout the day.
Caffeine, present in modest amounts, has a mild appetite-modulating effect as well. It temporarily increases energy expenditure and slightly suppresses early hunger cues without overstimulation. Unlike synthetic stimulants, green tea’s combination of caffeine and catechins produces a gentle, sustained effect that feels natural rather than forced.
Green tea also supports digestive efficiency. Some research suggests it encourages the liver and pancreas to process nutrients more efficiently, indirectly affecting satiety signals. When the body can extract nutrients effectively, appetite becomes more proportional to actual need rather than guessing what is missing.
Taste matters here too. Sipping green tea between meals can provide a sensory cue that reduces habitual snacking. Its subtle bitterness engages receptors that signal “enough” in ways sweet or bland foods do not. Combined with metabolic support, this makes green tea a versatile tool in a holistic approach to appetite regulation.
7. Berberine-Containing Herbs (Berberis species)
Berberine is a plant alkaloid found in several herbs like barberry, goldenseal, and Oregon grape. Its effects on metabolism are profound, particularly concerning glucose regulation and insulin sensitivity. Berberine activates an enzyme called AMPK, often called the “metabolic master switch.” This enzyme improves how the body processes carbohydrates and fats, smoothing out blood sugar fluctuations that drive erratic hunger.
Regular berberine use can reduce post-meal insulin spikes, preventing the crash that often triggers immediate, sometimes overwhelming hunger. By modulating glucose metabolism, it ensures that the energy coming from food is used efficiently, allowing appetite signals to reflect true nutritional need rather than reactive cravings.
Berberine also appears to have mild effects on gut microbiota. A healthy microbial balance supports the production of short-chain fatty acids and peptides that communicate satiety to the brain. In this way, berberine contributes to appetite regulation not only through metabolism but also through the gut-brain axis.
Because berberine is potent, it is most effective when paired with meals or taken in divided doses. It is not a “quick fix” for cravings but a tool that stabilizes hunger patterns over time. For anyone struggling with post-meal hunger that feels uncontrollable, berberine-containing herbs are among the most evidence-based options.
Together, these digestive and metabolic herbs illustrate a principle: when the internal systems that handle food, energy, and nutrient signaling are optimized, appetite naturally stabilizes. Ginger fine-tunes digestive mechanics. Green tea balances metabolic and sensory inputs. Berberine-containing herbs regulate blood sugar and gut signaling. Each targets a distinct lever in the complex machinery of hunger. When used consistently, they allow appetite to behave like it should—responsive, proportional, and reliable—without resorting to restriction or suppression.
By addressing both the mechanics of digestion and the chemistry of metabolism, these herbs provide a foundation on which true appetite control can be built. The body learns to recognize fullness, manage cravings, and respond appropriately to actual nutritional needs rather than reacting to chaos. It’s a subtle, slow, and deeply effective way to regain balance.
Medicinal Mushrooms and Nervous System Modulators of Appetite
Appetite is not just a matter of digestion and hormones—it’s profoundly influenced by the nervous system. Stress, fatigue, and emotional states can amplify hunger, suppress it, or make it unpredictable. This is where medicinal mushrooms shine. Unlike herbs that primarily affect metabolism or digestion, these fungi interact with the nervous system, immune signaling, and even the gut-brain axis to help regulate appetite naturally. They are subtle, patient modulators, not blunt instruments.
In traditional medicine, mushrooms were valued not for immediate suppression of hunger, but for restoring balance and resilience. They are calming, tonifying, and adaptogenic, meaning they help the body respond appropriately to internal and external stressors. This influence on systemic equilibrium often translates into steadier appetite patterns, especially for people whose hunger is linked to stress, fatigue, or inflammation.
8. Reishi Mushroom (Ganoderma lucidum)
Reishi is often called the “mushroom of immortality,” but its relevance to appetite is more practical than mythical. It modulates the autonomic nervous system, helping the body shift out of a constant “fight or flight” mode. Chronic sympathetic activation can exaggerate hunger or trigger emotional eating. By calming this response, Reishi allows hunger to become proportionate and rational.
Reishi also influences cortisol levels. Elevated cortisol drives both cravings and fat storage, particularly around the abdomen. Regular use of Reishi may help regulate cortisol production, reducing stress-induced hunger surges. People often notice they eat more mindfully, feel satisfied sooner, and stop reaching for snacks when anxiety or tension rises.
Another mechanism involves the gut-brain axis. Reishi contains polysaccharides that support gut microbiota balance. Healthy microbiota contribute to the production of signaling molecules that communicate satiety to the brain. When this communication is clear, appetite is more consistent, and cravings that stem from imbalance diminish.
Reishi is not stimulating, and it does not suppress hunger forcibly. Its impact is gradual and cumulative, usually felt over weeks of consistent use. For appetite control, it works best in combination with herbs or dietary strategies that support blood sugar and digestive function. The effect is a calm, steady hunger that reflects actual energy needs.
9. Cordyceps Mushroom (Cordyceps sinensis)
Cordyceps occupies a slightly different niche among medicinal mushrooms. It is renowned for supporting energy production and endurance, often used to combat fatigue and boost resilience. Fatigue is a major driver of irregular appetite. When the body is tired, it craves quick, often carbohydrate-rich sources of energy, overriding natural satiety signals. Cordyceps helps restore energy efficiency at a cellular level, reducing the need for compensatory eating.
Cordyceps also has mild adaptogenic effects, modulating the adrenal and nervous systems to respond appropriately to stress. This reduces erratic hunger caused by cortisol fluctuations. Users frequently report that they feel less compelled to snack out of stress or boredom, and that meals feel naturally satisfying.
Metabolic effects are another angle. Cordyceps supports oxygen utilization and ATP production, making energy metabolism more predictable. When energy is efficiently produced and used, the body sends accurate hunger signals. People often notice they eat less impulsively, not because of suppression, but because energy needs are being met more reliably.
In practice, Cordyceps is best used consistently, either as a daily extract, tea, or powdered supplement. Its effects are subtle but measurable: appetite becomes less reactive, and energy-driven cravings diminish, allowing true hunger to guide eating behavior.
10. Lion’s Mane Mushroom (Hericium erinaceus)
Lion’s Mane is remarkable for its neuroprotective and neuroregenerative properties. While it is most often discussed in the context of cognitive function, these effects have important implications for appetite regulation. By promoting nerve growth factor (NGF) and supporting neuroplasticity, Lion’s Mane can help the central nervous system respond to hunger cues more accurately.
Emotional eating, stress-driven cravings, and mindless snacking often have neurological roots. Lion’s Mane doesn’t suppress appetite but enhances the brain’s ability to process signals from the body. Hunger becomes a reliable guide rather than a distorted signal. People report greater clarity around when they are truly hungry versus eating out of habit, stress, or emotional need.
Lion’s Mane also indirectly supports digestive function via its influence on the vagus nerve and gut-brain communication. Polysaccharides in the mushroom support gut microbiota, which in turn modulates satiety signaling. Appetite begins to feel intuitive again. You eat when necessary, stop when full, and cravings that once felt overwhelming fade naturally.
Taken together, these medicinal mushrooms illustrate the nervous system’s central role in appetite control. Reishi stabilizes stress hormones and gut communication. Cordyceps improves energy efficiency, reducing compensatory hunger. Lion’s Mane enhances neuroplasticity and the brain’s ability to interpret bodily signals. Used consistently, they create a calm, reliable internal environment where appetite can function as it was designed.
For anyone whose hunger feels erratic, emotionally driven, or influenced by stress, mushrooms like these offer a restorative path. They are not quick fixes, but agents of balance, helping the body learn to trust its own signals again. Appetite regulation becomes a byproduct of overall resilience, energy efficiency, and neural clarity—a more sustainable and physiologically sound approach than suppression or force.
Relearning Hunger Without Fighting the Body
Appetite regulation is often framed as a battle: fight cravings, suppress hunger, or force yourself to stop eating. That approach rarely works for long. The body is smarter than that. Hunger is a communication system, not an adversary. The goal is to relearn how to listen to it, to trust signals, and to respond appropriately. Herbs for appetite control are most effective when they support this process rather than override it.
Relearning hunger begins with awareness. Observe patterns: what makes you hungry, what keeps you full, and how stress, sleep, and emotion influence your eating. Many people eat reactively without realizing it—snacking out of boredom, eating late at night, or finishing meals when satiety has already arrived. Paying attention reveals the difference between physical hunger and psychological triggers.
Herbs and mushrooms provide the scaffolding for this awareness. They calm overactive stress responses, stabilize blood sugar, and support digestion, making hunger cues clearer. Gymnema can blunt the pull of sweet foods, helping you notice genuine appetite. Fenugreek and Ginger slow digestion, giving fullness time to register. Reishi and Lion’s Mane enhance nervous system and gut-brain communication. When used together thoughtfully, these botanicals help hunger feel proportionate and manageable, rather than overwhelming or confusing.
Practical strategies reinforce the effect. Eating at regular intervals, prioritizing nutrient-dense meals, and including protein, fiber, and healthy fats all strengthen appetite regulation. Herbal teas or tinctures between meals can provide sensory cues and mild physiological support without adding calories. This combination allows the body to relearn fullness gradually, not through restriction, but through consistent, supportive signaling.
Mindfulness during meals also matters. Eating slowly, savoring flavors, and paying attention to physical sensations can recalibrate internal cues. Herbs enhance this process: the bitterness of Gymnema, the warmth of Ginger, or the subtle grounding of Reishi can make meals more satisfying, slowing the desire to overeat. Appetite becomes a guide rather than a challenge.
It’s important to respect natural fluctuations. Hunger varies day to day depending on activity, stress, and sleep. Herbs for appetite control do not create rigid patterns; they smooth extremes. Some days you may feel hungrier or less hungry, and that is normal. The goal is proportionality, not elimination.
Cravings deserve attention too. They often signal more than simple hunger: micronutrient deficiencies, emotional stress, or overstimulation from processed foods. Herbal allies can reduce compulsive cravings and allow these signals to be interpreted correctly. For example, Berberine stabilizes blood sugar, reducing sudden sugar cravings. Cordyceps enhances energy utilization, making cravings less urgent. Lion’s Mane helps the brain distinguish between emotional impulses and true physiological need.
Patience is essential. Appetite regulation is a process, not a quick adjustment. Herbs and mushrooms act gradually, supporting internal systems until hunger becomes reliable again. Many people notice improvements over weeks rather than days. Consistency in use and lifestyle habits compounds the effect.
Relearning hunger is also a practice in trust. Trust that fullness will arrive, that appetite signals are meaningful, and that occasional indulgence does not derail balance. Herbs assist by ensuring the physiological and neurological systems behind hunger are functioning optimally, creating a foundation for sustainable regulation.
Ultimately, this approach reframes appetite. It is not something to be fought or feared. It is a guide, a messenger of needs and energy. With herbs, mushrooms, and mindful habits, hunger becomes predictable, manageable, and informative. Eating stops being a source of conflict and starts being a cooperative dialogue between body and mind. By restoring trust in appetite, you achieve balance naturally, without restriction, suppression, or guilt.
Best-selling Supplements for Appetite Control
Article Sources
At AncientHerbsWisdom, our content relies on reputable sources, including peer-reviewed studies, to substantiate the information presented in our articles. Our primary objective is to ensure our content is thoroughly fact-checked, maintaining a commitment to accuracy, reliability, and trustworthiness.
- Saper, R. B., Kales, S. N., Paquin, J., Burns, M. J., Eisenberg, D. M., Davis, R. B., & Phillips, R. S. (2004). Heavy metal content of Ayurvedic herbal medicine products. JAMA, 292(23), 2868–2873. https://jamanetwork.com/journals/jama/article-abstract/199049
- Preuss, H. G., Bagchi, D., Bagchi, M., Rao, C. V., Dey, D. K., & Satyanarayana, S. (2004). Effects of a natural extract of (-)-hydroxycitric acid on weight loss. Diabetes, Obesity and Metabolism, 6(3), 171–180. https://doi.org/10.1111/j.1463-1326.2004.00328.x
- Chevassus, H., Molinier, N., Costa, F., Galtier, F., Renard, E., & Petit, P. (2009). Fenugreek seed extract selectively reduces spontaneous fat consumption in healthy volunteers. European Journal of Clinical Pharmacology, 65(12), 1175–1178. https://doi.org/10.1007/s00228-009-0711-4
- Sharma, N., Gupta, P. C., & Rao, C. V. (2012). Anti-obesity effect of Caralluma fimbriata extract in rats. Pharmaceutical Biology, 50(6), 765–772. https://doi.org/10.3109/13880209.2011.618205
- Thompson, J. L., Manore, M. M., & Skinner, J. S. (2006). Exercise and weight loss: A review of the evidence. Sports Medicine, 36(2), 119–134. https://doi.org/10.2165/00007256-200636020-00004
- Hursel, R., Viechtbauer, W., & Westerterp-Plantenga, M. S. (2009). The effects of green tea on weight loss and weight maintenance. Obesity Reviews, 10(5), 499–512. https://doi.org/10.1111/j.1467-789X.2009.00599.x
- Yin, J., Xing, H., & Ye, J. (2008). Efficacy of berberine in patients with type 2 diabetes mellitus. Metabolism, 57(5), 712–717. https://doi.org/10.1016/j.metabol.2008.01.013
- Wachtel-Galor, S., & Benzie, I. F. F. (2011). Ganoderma lucidum (Lingzhi or Reishi). In Herbal Medicine: Biomolecular and Clinical Aspects. CRC Press. https://www.ncbi.nlm.nih.gov/books/NBK92757/
- Zhu, J. S., Halpern, G. M., & Jones, K. (1998). The scientific rediscovery of an ancient Chinese herbal medicine: Cordyceps sinensis. Journal of Alternative and Complementary Medicine, 4(3), 289–303. https://doi.org/10.1089/acm.1998.4.289
- Mori, K., Inatomi, S., Ouchi, K., Azumi, Y., & Tuchida, T. (2009). Improving effects of the mushroom Yamabushitake (Hericium erinaceus) on mild cognitive impairment. Phytotherapy Research, 23(3), 367–372. https://doi.org/10.1002/ptr.2634
- Sangiovanni, E., Brivio, P., Dell’Agli, M., & Calabrese, F. (2017). Botanicals as Modulators of Neuroplasticity: Focus on BDNF. Neural Plasticity, 2017, 5965371. https://doi.org/10.1155/2017/5965371
- Panossian, A., & Wikman, G. (2010). Effects of adaptogens on the central nervous system and the molecular mechanisms associated with their stress-protective activity. Pharmaceuticals, 3(1), 188–224. https://doi.org/10.3390/ph3010188
- Khan, A., Safdar, M., Ali Khan, M. M., Khattak, K. N., & Anderson, R. A. (2009). Cinnamon improves glucose and lipids of people with type 2 diabetes. Diabetes Care, 26(12), 3215–3218. https://doi.org/10.2337/diacare.26.12.3215
- Gadde, K. M., Martin, C. K., Berthoud, H. R., & Heymsfield, S. B. (2018). Obesity: Pathophysiology and management. Journal of the American College of Cardiology, 71(1), 69–84.https://doi.org/10.1016/j.jacc.2017.11.011
- Plant-Based Iron, Iodine, and Mineral Support Using Herbs - January 23, 2026
- Vegan Alternatives to Beeswax and Honey in Herbal Preparations - January 22, 2026
- Alcohol Free Herbal Extracts, Glycerites, Vinegar Extracts, and Teas Explained - January 22, 2026